engorgement

Congestion manifests with pain and hard knots in the chest (© Jacek Chabraszewski)
Congestion is noticeable through a very painful, hard spot in the chest. The hard spot may be small or cover a larger area and will not soften by breastfeeding. As the milk builds up, hard nodules, milk-filled glandular tissue, are noticeable. The skin may be reddened over the affected area. Stagnation can promote infection with bacteria (see breast inflammation).
Causes and risk factors
In case of a milk congestion, the milk flow is mechanically impeded:
- through a Cuticle at the opening of a milk duct, as described under: white blisters on the nipple
- through a Fettpfropf. Fat usually settles between two nursing meals in the form of small globules on the wall of the milk ducts until a milk donor reflex rinses the fat globules towards the exit (nipples). When these globules clump together, a congestion occurs.
- In some mothers, white, sand-like granules were observed in the milk. It is believed that yourself Calcium granules in the breast milk and clog the milk ducts.
- It is also believed that dead cell clumps can clog the milk ducts.
Most likely, the Pfröpfe consist of a mixture of milk fat, dead cells and other solid milk components. The material usually dissolves during breastfeeding over time or is rinsed out. Sometimes such Pfröpfe are found directly on the nipple. When removed, they look like thickened spaghetti paste, sometimes brown, yellow or green in color. For the baby, the material is harmless.
The following risk factors increase the likelihood of a milk congestion:
- insufficient or rare emptying of the breast, e.g. if the child is prematurely removed from the breast before it is thoroughly emptied, or there is an unusually large break between nursing meals. The child may suddenly drink less, or not drink at all, e.g. distraction, travel, outside help, mother’s work or a strike strike.
- abundant milk production. The likelihood of a congestion is greatest in the first few weeks and months, where plenty of milk is produced, and lowest when an older infant or toddler drinks very little milk. If the mother makes more milk than her child drinks (see Too Much Milk), her risk of recurring milk congestion is increased.
- Impairment of the milk donor reflex e.g. through stress (visit, travel, time pressure, etc.), exhaustion, smoking or alcohol consumption of the mother. If the milk donor reflex of the mother is impaired, more milk remains in the breast, the baby gets less (see also If the milk donor reflex is blocked).
- The Stitching the breast by baby slings, pumping funnels or a restrictive bra, e.g. an unfavorably fitting underwired bra that constricts the breast tissue. Milk ducts may temporarily “stick together” under the pressure or collapse locally, so that the milk can not flow or flow through it less.
In summary, one “Milchstase“The formation of milk congestion. If milk remains in the breast, it is reabsorbed into the bloodstream over time. The milk may thicken and occasionally clump together. How the discharge in a milk duct is blocked (damming up).

The baby’s chin should point to the dammed place. If the congestion is in an upper segment of the breast, then the baby can be placed over his shoulder while breastfeeding. If an inner side of the chest is jammed, then the Wiegehaltung is good, with an outer segment, the football posture and a lower segment breastfeeding while lying down (Drawing: bearsky23).
treatment
The most important measure for the therapy of a milk congestion is the regular and thorough emptying of the breast. Often, the situation improves on its own if the baby is still breastfed frequently (for example every 1-3 hours). In addition, the milk can be obtained manually or with the help of a breast pump if the baby does not empty the breast sufficiently. It is also recommended, to start breastfeeding with the affected breast, to effectively empty this breast. In order to further promote effective emptying, the baby should be nursed so that his chin points to the affected area. The pull is strongest in this area.
In order to dissolve the clumping and to promote the milk flow, at the affected place a few minutes before breastfeeding or before the chest emptying warmth be applied, e.g. using a warm compress (not too hot to avoid scalding).
For pain relief, the nursing mother may Painkiller taking ibuprofen or paracetamol with the active ingredient, while you can continue breastfeeding (ask your doctor, pharmacist, midwife or lactation consultant).
When breastfeeding in fours Gravity supports milk flow.
After breastfeeding or emptying the breast will be refrigeration applications recommended: quark wrap or cold envelopes. The cold application should take about 20-30 minutes. The nipple should always be left out in a quark wrap, especially if the nipple is sore! Quark attacks the sensitive skin of the nipples and the baby should not eat any quark.
White cabbage leaves (rolled with a rolling pin before use) can be placed in the bra between breastfeeding meals. White cabbage leaves have an anti-inflammatory and cooling effect.
Trying to express the congestion by force, increases the risk of breast abscess. A breast massage should therefore be carried out very carefully and gently in the case of an existing milk congestion and must not hurt! It may be a very gentle massage in front the milk congestion, ie between the nipple and the milk congestion (and not Behind or at the Engorgement). If a graft obstructs the milk discharge, it lies in front the milk jam. You can start the gentle massage near the nipple and work your way slowly towards the jam. The tissue is gently moved to loosen and then stroked towards the nipple. The massage can be carried out under warm water e.g. be done under the shower.
If the exit of a milk duct at the nipple is blocked by a overgrown skin blister or fat plug, the duct may be blocked e.g. through under the warm shower Rubbing or careful manual removal can be reopened (do not squeeze!) (see white blisters on the nipple).
prophylaxis
In some women, excesses of milk (temporarily) occur again and again. To prevent further milk congestion, you can have your breast once a day massage under the warm shower and several times a day before breastfeeding, to solve any clumping and sticking. The Plata Rueda massage can be done in a matter of seconds so the baby does not have to wait.
Affected women should take care that their Breast is regularly and thoroughly emptied and no milk stasis arises. When the chest tenses, they can wake their baby to drink. If they are separated from their baby then they can empty their breasts manually or with a pump over time. When introducing complementary foods, they should not skip breast-feeding, but often continue breastfeeding and spread the supplement over several days (as recommended by the WHO). This way, complementary foods can be introduced in a breast-friendly way.
So that all segments of the breast are well emptied, the Stuck position alternated become.
If the milk accumulation occurs due to a temporary excess of milk, milk production can be reduced by cooling after breastfeeding. Cooling causes the blood vessels to contract and slow down all metabolic processes. It may take a few weeks during the first time after birth until milk production adapts to the needs of the baby.
Women who are prone to clumping milk fat may pay attention to the dietary intake of polyunsaturated fatty acids lecithin (Lecithin) in addition (for example, daily 1 to 4 tablespoons granules or 1-2 gastric juice-resistant capsules, each containing 1200 mg). Lecithin is an emulsifier that brings fat into solution, avoiding lumps of fat. In natural food, lecithin occurs in vegetable seeds and egg yolk. In industry, lecithin is mostly made from soya.
With recurring milk congestion can also probiotics for the lactating breast to be taken prophylactically (more in section Dysbiosis).
If there is an accumulation of milk over and over again in the same place, one can fibrocystic mastopathy (nodular augmentation of the breast connective tissue) or a tumor may be considered. In such cases, it is recommended to have yourself examined by a gynecologist. As a rule, these are benign breast changes.
Swell:
- Lawers J, Swisher A: Conseling the Nursing Mother. A lactation consultant’s guide. 6. On. 2016. p. 393-394.
- Walker M: Breastfeeding Management for the Clinician. Using the evidence. 4th edition 2016, pp. 605-606.
- Berens P, Eglash A, Malloy M, Steep A, Academy of Breast Feed Medicine: ABM Clinical Protocol # 26: Persistent Pain with Breastfeeding. Breastfeeding Medicine 2016; 11 (2).
- Kloster I: Stillmanagement in various still-life situations. Seminar of the Training Center Lactation & Breastfeeding, August 2019.
- S3 guideline for the treatment of inflammatory breast diseases during lactation 2013.
- Lawrence RA and Lawrence RM: Breastfeeding. A guide for the medical profession. 5th edition, 1999, Mosby and 6th edition, 2005, Elsevier Mosby
- Riordan J and Auerbach KG: Breastfeeding and Human Lactation, 2nd edition, 1999; Jones and Bartlett Publishers
Further online publications on the topic:
© Dr. Z. Bauer – Publications in breastfeeding. 2003-2019. Last revision: September 2019.
Related Posts
-

What is decubitus? Causes, symptoms, treatment »
bedsore Pressure ulcers – sore from lying Decubitus is an ulceration due to pressure. The strength of the pressure ulcer can be divided into 4 stages,…
-

Shingles in pregnancy: causes, symptoms and treatment
Shingles in pregnancy: information on causes, symptoms and treatment Responsible for the disease Shingles (also known as herpes zoster) is a virus that…
-

Sciatica pain in pregnancy: causes and treatment
Sciatic pain in pregnancy: causes and treatment methods Sciatic pain during pregnancy can be triggered by several causes. Already that Weight of the…
-
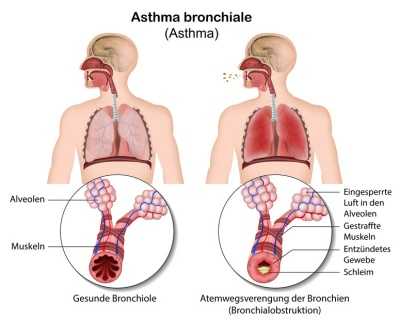
Bronchial asthma – causes, symptoms & treatment
bronchial asthma bronchial asthma or colloquial only asthma is a chronic inflammation of the respiratory tract. Cough attacks, shortness of breath and…
