Immunology, Regulation of dendritic cells

Dr. Dorit Fabricius Group
Immunology, Regulation of dendritic cells

University Medical Center Ulm
Department of Pediatrics and Adolescent Medicine
Research Lab, House 16
Eythstr. 24
89075 Ulm
germany
Tel .: + 49-731-500-57255
Fax: + 49-731-500-57042
Research Profiles
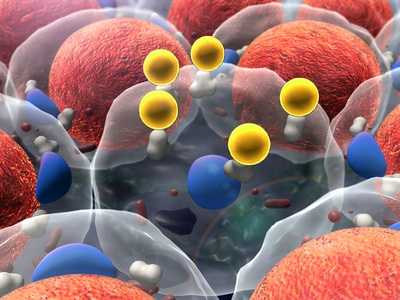
Plasmacytoid dendritic cells (pDC) are crucial mediators of innate and adaptive immune responses. A better understanding of pDC regulation may improve immunotherapeutic approaches to cancer, infectious diseases and autoimmunity. Apart from production of IFN-alpha and TNF-alpha, we have found that pDC can secrete large amounts of the serine protease granzyme B (GrB), but no perforin. In the last years we investigated the regulation of GrB in pDC based on our finding that pDC-GrB effectively suppresses T cell proliferation. While the cytokines IL-3 and IL-10 played a key role in GrB induction, toll-like receptor agonists and CD40 ligand inhibit GrB secretion. To denote the physiological function of pDC-GrB, we have exploited the effect of commonly used antiviral vaccines on pDC allowed for an efficient cell response. TBEV vaccination produced less than before vaccination, as well as contributing to a successful cellular immune response to the vaccine. Grb-secreting pDC in suppression of tumor-specific cells and suggesting that pDC can have a regulatory role, mediated by GrB in the absence of perforin; a mechanism that has been described for regulatory T cells. Since IL-3 and IL-10 can also be found in the environment of malignant tissues, pDC-GrB may be involved in suppression of tumor-specific T cells. Interestingly TBEV was used in a tumor vaccination study as a natural agonist and we assume the suppression of GrB contributed to the observed anti-tumor effect. Model of immune responses against B cell leukemias. By including pDC from healthy subjects and patients with B cell leukemias, we hope to achieve a better understanding of the role pDC play in health and disease and how this potent immunomodulating cell population may be manipulated therapeutically.
Acute lymphoblastic leukemia (ALL) is the most common pediatric malignancy. 20% of cases and have a poor prognosis. Thus, novel therapeutic strategies are required to treat minimal residual disease and improve long-term survival. The CpG oligodeoxynucleotides (CpG) can induce immunogenicity of non-Hodgkin’s lymphomas including B-CLL and in certain B cell leukemias. B cell stimulators, including CpG, interleukin (IL) -2 family cytokines and CD40 ligand (CD40L) on the immunogenicity of BCP-ALL cells, could be shown to be the combination of CpG, IL B-Cells and Buffering Cells: BCP-ALL Cells and Induced Cells Cytotoxic T Cells (CTLs). Often, these CTLs exhibited significantly enhanced anti-leukemic cytotoxicity, not only toward but also untreated BCP-ALL cells. Untreated control of BCP-ALL cells induced only minimal T cell proliferation and cytotoxicity even in allogeneic setting. Our results demonstrate that combined treatment with CpG, IL-2 family cytokines and CD40L is more efficient than CpG alone in inducing immunogenic phenotype in BCP-ALL cells. Anti-leukemic immunity would be characterized by additional stimulation of tumor-lysate-loaded activated pDC and the role of pDC in an in vitro CTL generation. Apart from in vitro studies we want to use a humanized leukemia mouse model that will be transplanted with BCP-ALL. In this xenotransplantation model, we aim to test the anti-leukemic immune response of vitro in vitro generated specific CTL. The planned in vivo study may provide novel insights in mechanisms of immunogenisation and contribute to the development of immunotherapeutic vaccination approaches in the management of therapy-resistant BCP-ALL.
Related Posts
-

Experimental anesthesiology – university hospital ulm
Our profile What we do The Section Experimental Anesthesiology of Prof. dr. E. Marion Schneider pursues monocytes and immature dendritic cells in septic…
-
Cell metabolism – function, task & diseases
Cell metabolism Of the Cell metabolism is the basis of all vital and biochemical processes in the body that take place inside and outside a cell….
-

Regeneration research in diabetes: future application
Regeneration Research in Diabetes: Future Application Areas Therapies with stem cells Stem cells are the hope of modern medicine. Into the one hand they…
-

Regeneration research in diabetes: basics
Regeneration Research in Diabetes: Basics Beta cells and islets of Langerhans The beta cells are the insulin-producing cells in the pancreas. They are…
