X-leg or valgus knee is a malalignment of the leg, in which the hip has an adduction position (the knee shifts inwards) and internal rotation: with parallel thighs, the ankles move apart.
In the first 18 months of life, the knee is in the varus position (outward).
This misalignment can also often be seen in football players.

In children between 18 and 24 months, the joints of the hips, knees and ankles are normal or straight (the legs are parallel). If the child is between 2 and 5 years old, a valgus position (inwards) is normal. Then the knees are neutral again.
This deformity is more common in girls, but boys can develop it too.
It usually occurs bilaterally, so it is present in both knees.
The malformation can be seen when the child is 2 or 3 years old and may worsen until the age of 4.
The valgus position of the knees can correct itself by the age of 7 or 8. The malposition rarely persists until adolescence.
Before the age of 6, the child should undergo a medical examination, otherwise bone malformations (pathological valgus position of the knees) may remain.
The malformation can become serious.
Overweight damages the knee joints and can cause problems with Go to lead.
Complications and consequences
Usually, young people have no problems, but adults or the elderly can show wear on the outside of the cartilage and meniscus. This could result in arthrosis, especially in the lateral knee area.
Why is there a valgus position in the knee joint? What are the causes of the valgus knee?
Studies confirm that the valgus knee is caused by four specific factors.
The four causes are listed below, in order of most likely to less likely.
1. Lack of strength in the pelvis
Muscle weakness in the buttocks (small buttock muscle, medium gluteus muscle, large gluteus muscle and external rotators of the hip) together with increased muscle tone of the abductors prevents the stabilization of the thigh bone. The flanks shift inwards and the hips turn inwards. If the abductors are stronger than the external rotators (gluteus / hip), the knee will get a "pull" in the valgus position.
2. Ankle stiffness
The reduction in dorsiflexion (lifting of the toes) of the upper ankle and the muscle weakness of the gastrocnemius, soleus and tibialis anterior prevent the leg extension for correct walking. This leads to pronation of the feet (the foot turns outwards and the ankle turns inwards). This results in an internal rotation and adduction of the hip. The result is an X-leg position.
3. Quadriceps weakness
When the vastus medialis muscle is weak, it does not stabilize the knee. This leads to a "squinting" patella (the kneecap looks outwards) and the knee tends inwards, i.e. into a valgus position.
4. Weakness of the ischiocrural muscles
Weakness of the middle and back muscles of the thigh (M. semimembranosus and M. semitendinosus) does not allow stabilization of the knee joint. The joint "shifts" to the middle (similar to what happens to the inner thigh muscle), but on the back page of the thigh.
The knee joint experiences a combination of these factors, but if a malposition develops, it is not only an orthopedic disorder (muscle strength and flexibility), but also a problem of annoy.
There are other factors that favor an X leg?
Anatomy plays an important role in the valgus knee. Factors that affect this knee position are:
- Beck width
- Angle of the acetabulum (part of the pelvis where the femur enters)
- Shape of the femur
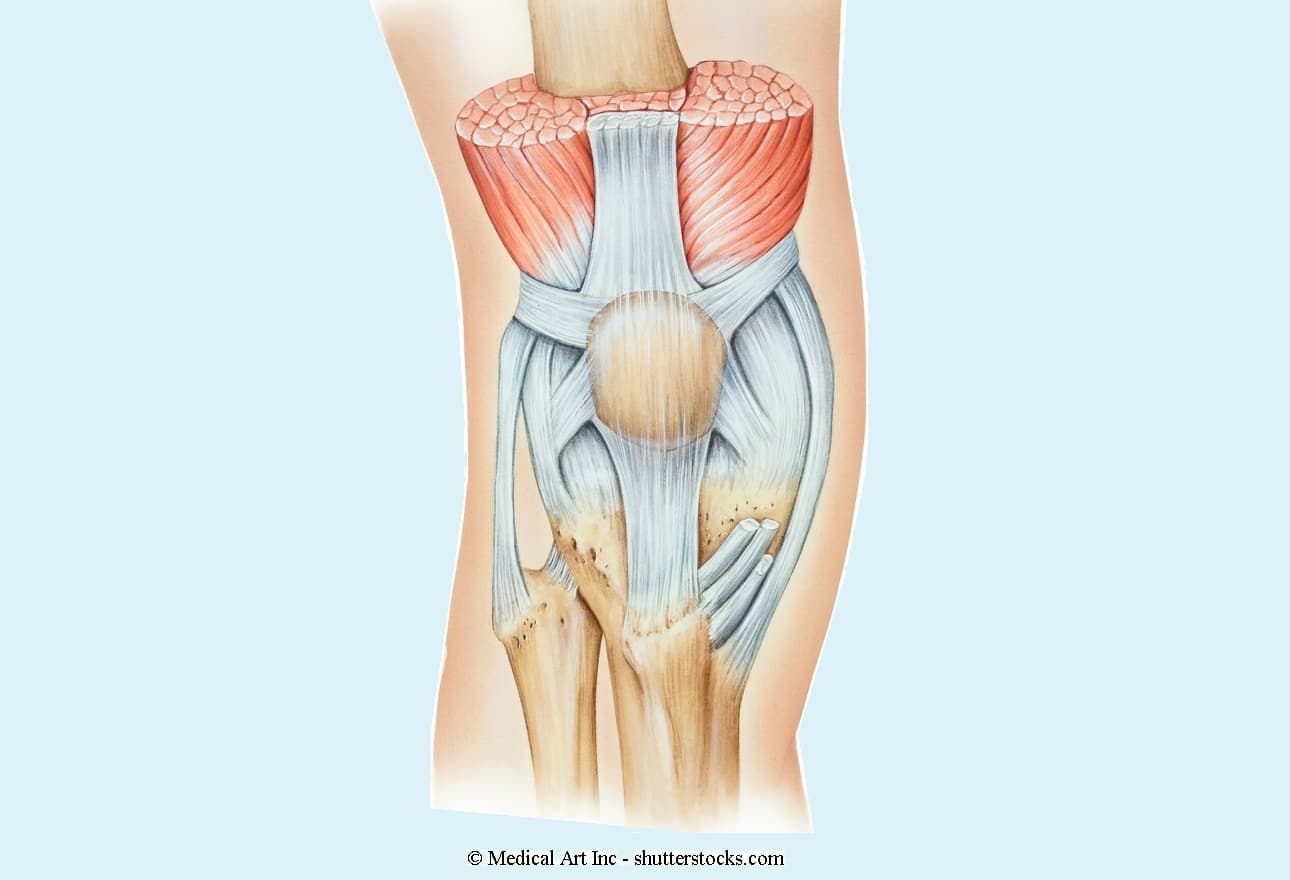
- Structure of the knee joint
- Course of the tibia
- Ankle shape
- Size of the foot
- Laxity of the ligaments
Some people are more prone to X-leg formation.
As I said, the valgus knee is caused by a loss of strength in the hip or reduced mobility in the ankle.
Symptoms of the valgus knee
The X-leg position is usually asymptomatic for many years. But over time, it can cause knee pain indoors.
The patient walks with their knees close, but if there is a valgus knee on only one side (monolateral), the back is misaligned and swings from one side to the other.
The stability of the knee joint is reduced.

Knock-knees
© Massimo Defilippo
Diagnosis of the valgus knee
The severity of the valgus position in the knee joint is determined by measuring the intermalleolar distance (distance between the ankle joints) with the knees closed.
- Degree (physiological) up to 2.5 cm
- Degree (easy degree) between 2.5 and 5 cm
- Degree (moderate) between 5 and 7.5 cm
- Degree (highly) over 7.5 cm
What to do? How are X-legs treated??
Among the natural remedies there are corrective exercises for the gym or at home:
1st exercise
The patient lies on the side of the affected knee joint. He bends his healthy knee to the right angle and supports the foot in front of the valgus knee, then he stretches the lower leg, the foot must be in the hammer position.
Then lift the leg lying on the floor, keep it straight (you can feel the effort on the inside of the thigh). 10-12 repetitions, then leg changes.
2nd exercise
Perform an adduction of the legs (move the knees towards each other) while sitting on a chair with a ball. Position the ball between your knees and squeeze your legs firmly.
Do 10 repetitions.

3rd exercise
The exercise begins lying down (supine). Raise both legs, knees together and straight. As soon as they form a right angle with the back, open and close the legs. Perform 10-12 repetitions and rest for 30-40 seconds. Repeat the exercise 3 times.
4. Exercise
This exercise is similar to the previous one. You start on your back and raise one leg. It is best to bend the other leg so as not to put excessive strain on the back. With the leg raised, 5-8 circles are now made clockwise (as if you were drawing an O) and 5-8 circles counter-clockwise. Put the leg down and repeat the same exercise with the other leg.
Avoid exercises to strengthen the muscles of the outer thigh (abductors) if possible.
To the allowed sports include cycling (cycling) and swimming with moderate intensity.
Jogging is not recommended for a high-grade valgus position.
The orthopedist sometimes prescribes a rigid knee brace to keep the joint in its axis, but the child (or the adult) does not tolerate it for a long time.
The doctor may recommend insoles that support the foot and improve the alignment of the knee joint.
Osteopathy is a manual form of therapy that can improve the alignment of the knee by relieving existing muscle tension and unblocking the joints.

Surgical intervention
When to operate?
If the valgus position is greater than 8 °, the orthopedist recommends surgical intervention.
osteotomy
Among the hallux valgus solutions, the proximal (high) osteotomy of the shin aligns the knee joint and increases strength.
Wedge osteotomy is an open surgical procedure that has been used for 30 years. The surgeon removes a lateral bone wedge from the tibia.
In recent years, wedge osteotomy has been performed using resistant mounting plates. The doctor cuts the tibia, straightens the knee and fills the “emptiness” that has arisen with autologous (iliac crest) or synthetic material (hydroxyapatite).
This technique preserves the anatomy of the proximal tibia and bone tissue. This allows future knee prosthesis surgery and more accurate joint correction. And finally, it prevents injury to the peroneal nerve and the femoropatellar joint.
HTO technique
The patient is positioned supine and the procedure is prepared. The menisci and articular cartilage are assessed using arthroscopy.
During the surgical procedure, the surgeon makes a vertical incision over the base of the pes anserinus between the medial edge of the patellar ligament and the rear edge of the tibia (tibia).
The sartorius muscle is incised to expose the biceps femoris.
A "guide wire" is inserted into the proximal part of the tibia from the inside out. The guide wire is positioned at the level of the tibial tubercle and penetrates it obliquely by about 1 cm.
The guidewire ends under the joint line (space between the two bones) on the side of the shin.
The osteotomy is continued with a surgical saw by following the guidewire to prevent articular fracture. Shortly before the osteotomy is completed, the doctor fixes the 2 wedges with screws.
The guidance ensures that the part of the shin that carries the weight of the body is not cut.
The plate is fixed in the upper part with 6-7 mm long screws and in the lower part with 4-7 mm long screws.
The iliac crest or synthetic substrate is inserted into the wedge opening to avoid pseudarthrosis or delays in healing.
Postoperative course
The hospital stay in the orthopedic department lasts 2-5 days.
The internal fixation allows the patient to start the physiotherapeutic exercises and rehabilitation immediately and enables a quick recovery. The range of motion is sufficient to begin strengthening.
The physiotherapist mobilizes the leg the day after the operation.
Passive / active mobilization on the straight leg is started. The orthosis is removed on the second day. From there you can stretch your leg.
Rehabilitation exercises
At the beginning, the physiotherapist performs passive movements, but the patient has to work actively as soon as possible.
In the last part of the rehabilitation, it is common to strengthen the muscles with aids: leg press and leg curl.
In the first 3 weeks, the rehabilitation should be done without weights. These should only be used after an X-ray check.
The person begins walking without walking aids at the end of the third month.
If the rehabilitation is carried out correctly, the muscles are strengthened and stretched, while coordination and walking are improved.
RELATED ITEMS
-

Elbow fracture, surgery and rehabilitation exercises
What is an elbow fracture? An elbow fracture is the rupture or injury to at least one of the bones that link the joint…
-

Strengthening self-confidence in children – exercises and tips
Many children also learn during the holidays – this is shown by a scoyo survey. But parents find it even more important that children take their time off school…
-

7 exercises to learn to make fun for the children
If your child is currently learning to read, you can help them with these 7 learning exercises. Learning exercises to read are a great way,…
-

Muscular dystrophy in children, neurological disease (neurology), myopathy (muscle atrophy)
Childhood – it’s time to play and carefree. Oh, life isn’t all kids are so rosy: kids with muscular dystrophy just aren’t in…
